Kat KelleyGHTC
Kat Kelly is a senior program assistant at GHTC who supports GHTC's communications and member engagement activities.
Since its discovery in 2012, cases of Middle East Respiratory Syndrome (MERS)—a disease World Health Organization (WHO) Director-General Dr. Margaret Chan called “a threat to the entire world”— have been reported in 27 countries across four continents. MERS is a type of coronavirus (MERS-CoV)—a common virus that infects the nose, sinuses, and throat—and a close cousin to the Severe Acute Respiratory Syndrome (SARS), infamous for infecting more than 8,000 in the early 2000s. As its name reveals, MERS is a respiratory illness, however, the symptoms are non-specific, and include coughing, sore throat, fever, chills, and muscle pain. The disease can quickly turn into pneumonia, and more than one-third of cases are fatal.
History of MERS outbreaks
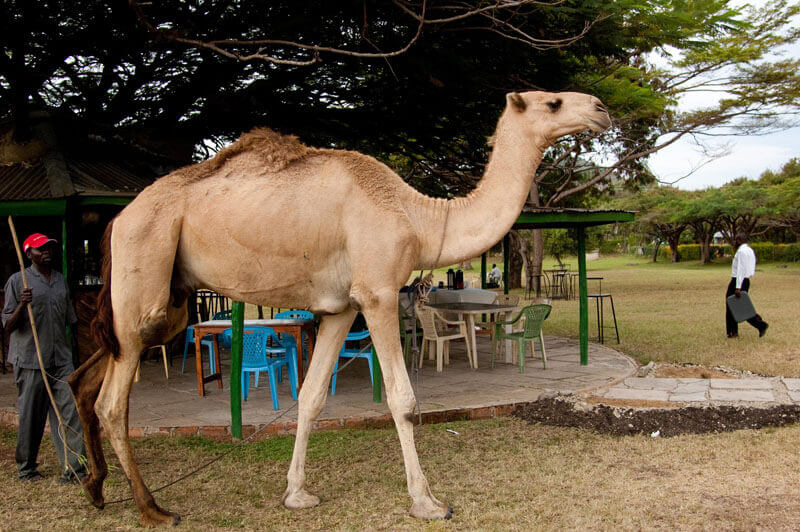
The virus is believed to have passed from bats to camels, and within the last few years, from camels to humans. To date, there have been more than 1,400 lab-confirmed cases resulting in nearly 500 deaths, primarily in the Arabian Peninsula. For the first time since its discovery, a major outbreak has occurred outside of the Middle East, with 186 cases and 36 deaths in South Korea in recent months.
MERS is not particularly contagious. One study from a spring 2014 outbreak in the Middle Eastsuggests that the average MERS patient—outside of a hospital setting—spreads the disease to just one other person. However, the Korean outbreak paints a different picture. Just one man is believed to have spread the disease to more than 20 people. Coronaviruses are particularly adept at mutating, and scientists initially feared that the virus had mutated to become more virulent. While an examination of genetic material from the Korean outbreak debunks this theory, the threat of mutation remains a real possibility.
"The fact that MERS has spread around the world is not surprising. The question is, 'Where is it going to spread to next?' It could very easily come to America. Very easily. Any flight could contain someone who was infected in the Middle East."
Michael Osterholm, director, Center for Infectious Disease Research and Policy, University of Minnesota
Status of MERS R&D
According to Ripley Ballou, vice president of Emerging Diseases at GlaxoSmithKline—the sixth largest pharmaceutical company worldwide—“everybody knows what the target for MERS is, it is the core spike protein […] a single protein that can be used to induce an immune response.” Despite this knowledge, there are currently no vaccines or drugs to prevent or treat MERS, and no large pharmaceutical companies have invested in MERS research & development (R&D). In the case of diseases with sporadic outbreaks, investments in R&D can be risky for pharmaceutical companies; if the outbreak is contained, there may no longer be a commercial market for the finished products. However, as Dr. Adrian Hill, director of the Edward Jenner Institute for Vaccine Research at Oxford University, points out “there is no sign of MERS going away. It’s been around since 2012.” The disease is endemic to Saudi Arabia and Hill argues the government of Saudi Arabia could afford to fund MERS R&D.
Currently, several small biotech companies and academic institutions are engaged in preclinical research for experimental MERS vaccines and drugs. Below GHTC examines the current R&D pipeline for MERS:
Vaccines
Greffex, Inc., a biotech company that specializes in the rapid development and production of vaccines, created an experimental vaccine for MERS in 2013, which was tested on mice the following year by the US National Institute of Allergy and Infectious Diseases (NIAID). Within just two months, Greffex produced and tested the vaccine and a complementary booster shot, which resulted in the production of protective antibodies—proteins developed by the immune system to fight a specific virus—in every single mouse. Greffex CEO John R. Price believes the company could produce a stockpile of vaccines for human clinical trials for “pennies on the dollar” in just three weeks, however the company could not afford costly clinical trials.
“How long are we going to wait around and just follow these outbreaks before we get serious about making vaccines?"
Adrian Hill, professor and director, Edward Jenner Institute for Vaccine Research, Oxford University
Dr. Matthew Frieman, a professor of Microbiology and Immunology at the University of Maryland School of Medicine, partnered with Novavax, Inc. to develop and test another experimental vaccine for MERS. This candidate also triggered the production of antibodies in mice and was tested in conjunction with a booster, and similarly, progress has ground to a halt, due to the lack of funding for clinical trials. “There's nothing standing in our way from pushing this forward other than the money and the will to do it,” Dr. Frieman told the International Business Times.
Fortunately, human clinical trials are planned for a third candidate, developed by a team of researchers at the Ludwig Maximilian University of Munich, thanks to funding from the German Center for Infection Research. Rather than using antibodies against MERS-CoV, this vaccine triggers the recipient’s immune system to produce its own antibodies against the virus by introducing a weakened poxvirus that has been genetically altered to express the characteristic MERS-CoV spike protein. The body recognizes the poxvirus as foreign, and develops antibodies against that spike protein, without ever seeing the MERS virus itself.
While three different vaccine candidates may seem like a foolproof defense against an outbreak, the work has only just begun. Clinical trials are not only expensive, but can take years to complete. For example, the US National Institutes of Health (NIH) announced the success of an Ebola vaccine in monkeys as early as 2000 and initiated a human clinical trial in 2003. However it wasn’t until 2006 that the results were published. While the vaccine seemed safe and effective, research ground to a halt until the recent Ebola outbreak in West Africa, and clinical trials continue to this day.

Drugs
Outbreaks are unpredictable, and given the costs and difficulty of vaccinating the entire world against MERS, treatment options are absolutely critical for this disease that kills more than one-third of those infected.
In South Korea, two hospitals are testing an experimental treatment for MERS known as convalescent plasma therapy, which uses blood plasma from survivors of the disease to boost the immune response of a current patient. The technique was also tested in the ongoing Ebola outbreak in West Africa and the 2000-2003 SARS outbreak in southern China. During the SARS outbreak, it decreased mortality by 23 percent. Plasma therapy is fast and inexpensive, and while it isn’t “medically proven” it’s “often carried out in the absence of other treatments,” a representative of the Hallym University Medical Center told The Korea Times.
In addition to his vaccine research, Dr. Frieman has partnered with Regeneron Pharmaceuticals Inc. to search for a treatment for MERS. The researchers genetically modified mice so that their cells would display the human version of a receptor protein—known as DPP4—to which the MERS virus attaches during an infection. This allowed them to mirror the human immune response to the virus. The team then examined more than 1,000 antibodies from the immune systems of the mice and tested the ability of those antibodies to prevent the MERS virus from latching on to human cells (via the DPP4 receptor). Left with 30 promising antibodies, the team needed to find two different antibodies that would not compete against each other and could be paired together, thereby producing a treatment that would be more effective against the mutability of the virus because it contained two different antibodies. The team identified two such antibodies that could work together, known as REGN3051 and REGN3048.
Dr. Frieman is also exploring the possibility of using drugs which are approved for other conditions to treat MERS. With NIAID funding, Frieman tested 290 different compounds, 27 of which were active against MERS-CoV in test tubes. The team will next examine the efficacy of these compounds in combatting MERS-CoV in mice. Several of these compounds are the basis of treatments for cancer or psychiatric conditions; similarly, Zoloft and Vascor—drugs for depression and angina, respectively—have been shown to be effective in combatting Ebola in mice.
Scientists at Purdue University have discovered a certain enzyme that plays a key role in the replication of the MERS virus, calling it the “Achilles’ heel of the virus.” They have since identified molecules that can stop the enzyme, making it much harder for the virus to replicate. However, that same molecule actually helped the virus spread at low doses, so determining the perfect amount of the molecule to administer will be a major barrier to translating their findings into a safe and effective treatment.
Other treatments are in development as well. Shanghai Kaibo Pharmaceutical plans to unveil an injectable treatment for MERS, however no information on the product has been released. Researchers at Fudan University in Shanghai, China have partnered with the NIH to develop an antibody against MERS known as m336 that they believe is even more promising than other antibodies against the virus.
As with vaccine candidates, the search for drugs and treatments against MERS is far from over. Not only do vaccines, medicines, and other tools need to be tested in clinical trials, but they need to be manufactured and distributed in adequate quantities to ensure a rapid response to an outbreak. Since its discovery in 2012, MERS has been widely considered a contender for the next major outbreak, or even pandemic. Researchers and public health advocates alike are wondering: will we learn from the Ebola outbreak and invest in R&D to create the tools needed to respond to a MERS pandemic, or will we wait until it’s too late?